Skin cancer is the most common, deadly form of cancer in the United States, but a study published in the Journal of Clinical Oncology says a modified version of herpes may be viable answer.
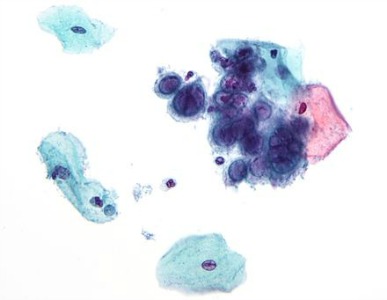
The treatment, T-VEC, is a genetically engineered version of herpes simplex virus type-1 that is injected into melanoma cancers.
Kevin Harrington, a professor of Biological Cancer Therapies at the Institute of Cancer Research in London, led the UK research team in the T-VEC study.
He found that the treatment not only killed cancer cells, but it stopped tumors from growing and helped strengthen the immune system against future cells.
Compared to chemotherapy, which can cause a number of side effects including chemo brain and hair loss, “...the viral treatment [T-VEC] can target cancer cells specifically...it tends to have fewer side effects than some of the other immunotherapies,” Harrington said.
More than 400 patients with aggressive, deadly melanomas were studied during this trial.
Those with stage III and stage IV melanomas that were considered inoperable lived twice as long as patients with earlier stages of melanomas who were using more traditional treatment.
The treatment has been engineered so it will not become an active herpes infection, as that can be deadly to cancer patients.
More than 70,000 Americans are diagnosed with melanoma each year and 10,000 are expected to die this year.
Scientists have been studying and testing cancer treatments using viruses as therapy, called immunotherapy, for several years.
T-VEC is the first immunotherapy to show evidence of benefiting the disease during phase III of a clinical trial.
This is significant because phase III is the last step in human testing before a drug can qualify for the approval of the Food and Drug Administration.
It should be noted that Amgen, the manufacturer of T-VEC, sponsored the study.
However, the results yielded from the research looks promising and many medical experts are singing T-VEC’s praises.
The treatment awaits FDA’s approval.
To learn more about T-VEC here:
http://www.medscape.com/viewarticle/814740