Click here to download the printable PDF version of the chart
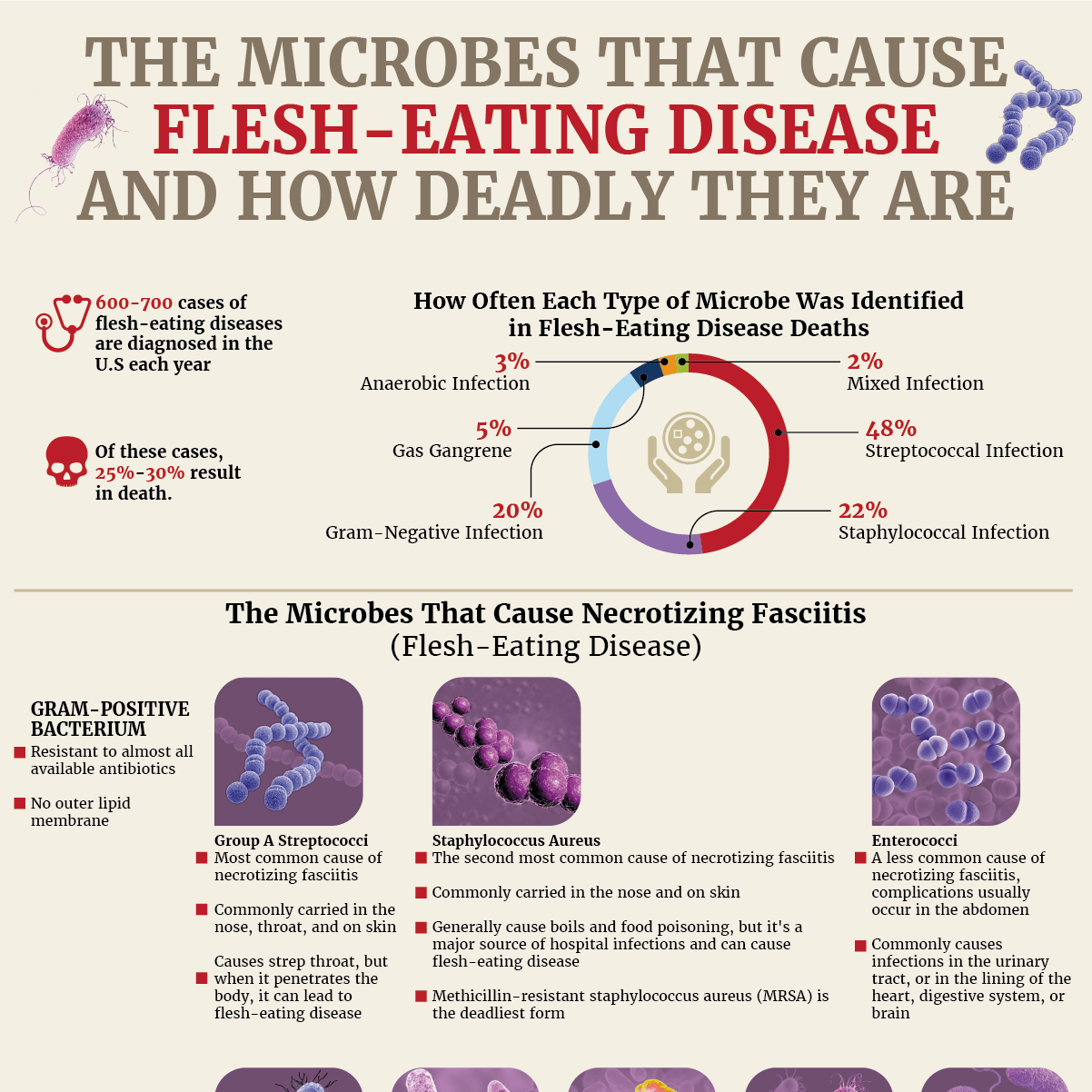
Flesh-eating disease: Just the name alone is enough to send shivers down your spine. But what causes it to develop, and how often are people diagnosed with this horrific condition? You may be surprised to learn that the flesh-eating bacterium that is known to cause necrosis or gas gangrene may be on your skin or in your nose at this very moment. It turns out that the strep bacterium that causes an annoying and painful strep throat is the same microbe that is responsible for causing the most cases of flesh-eating disease.
Read on to see which types of skin-eating bacteria, as well as a certain type of fungus, are responsible for the hundreds of cases of necrotizing fasciitis that occur each year in this infographic from NYRequirements.com.
What Is Flesh-Eating Disease
Flesh-eating disease, also known as necrotizing fasciitis, is a rare bacterial skin infection that can spread quickly throughout the body and be fatal. Certain types of bacteria have been found to cause necrosis. The microbes that cause flesh-eating disease can enter the body through surgical wounds, burns, minor cuts and abrasions, puncture wounds, or an internal organ that has been perforated or punctured, especially if this occurs in the colon, rectum, or anus, where quite a few of these microbes can naturally be found. Even insect bites can be an entryway for these dangerous strains of flesh-eating bacteria. A case involving necrotic tissue will need rapid treatment that includes antibiotics for skin infection, surgery, and sometimes even amputation of the infected body part.
Which Microbes Cause Flesh-Eating Disease?
The microbes that cause flesh-eating diseases include strains of Gram-positive cocci and Gram-negative rods, both of which have defenses that make them resistant to most antibiotics. Necrotizing fasciitis can also be caused by strains of anaerobic bacteria, which live and grow in environments without oxygen, so they can thrive in injured tissue deep within the body that doesn't have access to oxygen-rich blood. Certain microbes that fall under these three types are responsible for most cases of flesh-eating disease, which can be categorized as Type I or Type II depending on whether the infection is polymicrobial or monomicrobial. The nine microbes that most commonly lead to necrosis can be found below.
Gram-Positive Cocci
- Group A streptococci (Streptococcus pyogenes)
- Staphylococcus aureus
- Enterococci (Enterococcus faecalis)
Gram-Negative Rods
- Escherichia coli (E.coli)
- Klebsiella pneumoniae
- Prevotella
- >Pseudomonas aeruginosa
Anaerobes
- Bacteroides
- Clostridium species (Clostridium perfringens, Clostridium septicum, Clostridium sordellii)
On rare occasions, necrotizing fasciitis can also be caused by a bacterium found in saltwater called Vibrio vulnificus, which causes what is considered to be a Type III infection. It can enter the body through a cut or abrasion on the skin while swimming in infected water or be ingested through raw or undercooked seafood. This microbe has a mortality rate of 30% to 40% and is most commonly found in the Gulf of Mexico.
The last type of flesh-eating infection is fungal in nature, though this is a very rare cause of the disease. The Mucoralean fungi can cause a skin infection to turn into necrotic tissue, especially in patients who are immunocompromised.
Which Flesh-Eating Bacteria Is the Deadliest?
The deadliest flesh-eating bacteria is Group A streptococci (Streptococcus pyogenes), which is the most common form of bacteria that causes necrotizing fasciitis. Streptococcus bacteria has been identified in 48% of necrotizing fasciitis-related deaths that were determined with a microbiological diagnosis. It is the same bacteria that causes strep throat and is commonly carried in our noses and throats and on our skin without any symptoms. It’s when this form of bacteria penetrates through the skin barrier into the body that it can cause a necrotic wound. The speed and deadliness of this infection accelerates if it occurs in conjunction with streptococcal toxic shock syndrome (TSS).
Most Common Microbe in Necrotic-Fasciitis-Related Deaths
- Streptococcal infection: 48%
- Staphylococcal infection: 22%
- Gram-negative infection: 21%
- Gas gangrene: 5%
- Anaerobic infection: 3%
- Mixed infection: 2%
How Common Is Necrotizing Fasciitis (Flesh-Eating Disease)?
Necrotizing fasciitis is not a common type of skin infection; it occurs at a rate of 0.4 per 100,000 people. Of the 600 to 700 cases of flesh-eating disease that are diagnosed in the United States each year, 25% to 30% of them will result in death. The incidence rate increases with age; patients 80 and older are diagnosed at a rate of 12 per 100,000, while children are diagnosed at a rate of 0.08 per 100,000. According to our findings, nearly 70% of necrotizing-fasciitis-related deaths occurred in patients 55 and older.
Thankfully, necrotizing fasciitis symptoms are rare to see in a skin infection. To protect yourself from a skin infection developing into necrotic tissue or gas gangrene, be sure to clean any cut, scrape, or wound, no matter how small. If the skin around a wound becomes red, swollen, painful, or hot, be sure to get it checked out by a medical professional.
How Often Each Type of Microbe Was Identified in a Microbiologic Diagnosis of Necrotizing Fasciitis-Related Deaths
- Streptococcal Infection: 48%
- Staphylococcal Infection: 22%
- Gram-Negative Infection: 20%
- Gas Gangrene: 5%
- Anaerobic Infection: 3%
- Mixed Infection: 2%
The 4 Types of Necrotizing Fasciitis
Type I Infection
- Polymicrobial, caused by a combination of Gram-positive, Gram negative, and anaerobic bacterial types; an average of four different organisms are usually identified.
- 70-80% of cases.
- Usually affects abdominal or groin area.
- It typically affects older people with a comorbidity, such as diabetes mellitus, obesity, or immunodeficiency. Additional risk factors can include infection due to insect bites, surgical incisions, indwelling catheters, IV drug use, or alcohol abuse.
- Mortality variable depending on underlying health issues.
Type II Infection
- Monomicrobial (caused by a single type of bacteria), most commonly group A streptococci. It can occur with or without a coexisting staphylococcal infection.
- 20-30% of cases.
- Usually involves the extremities.
- Commonly affects young, healthy adults with a history of recent trauma or operation to the affected tissues.
- Mortality >32%, especially if associated with TSS.
Type III Infection
- Caused by Vibrio vulnificus, a bacterium found in saltwater that enters through an injury in the skin while swimming in infected water or by eating raw or undercooked seafood
- Rare type of infection, most commonly found in the Gulf of Mexico
- Mortality 30-40%
Type IV Infection
- Fungal in nature, with the mucoralean fungi emerging as a cause of skin infections that can form into necrotizing fasciitis
- A very rare type of infection, found to commonly affect patients who are immunocompromised or those with traumatic wounds or burns
- Mortality >47%, especially if immunocompromised
How Common Is Necrotizing Fasciitis?
- Every year, between 600 and 700 cases are diagnosed in the U.S. (a rate of 0.4 per 100,000 people per year).
- Of these cases, 25%-30% result in death.
- The incidence rate increases with age:
- Subjects 80+ years old have a rate of 12 per 100,000.
- Children have a rate of 0.08 per 100,000.
Percent of Necrotizing Fasciitis-Related Deaths by Age
- < 1 year old: 0.3%
- 1-4 years old: 0.1%
- 5-14 years old: 0.3%
- 15-24 years old: 0.7%
- 25-34 years old: 3.0%
- <35-44 years old: 8.0%
- 45-54 years old: 19.0%
- 55-64 years old: 24.9%
- 65-74 years old: 19.2%
- 75-84 years old: 16.1%
- > 84 years old: 8.3%
How the Microbes That Cause Necrotizing Fasciitis Can Enter the Body
- urgical wounds
- Puncture wounds or other injuries
- Burns
- Minor cuts
- Insect bites
- Abrasions
- Punctured/perforated internal organs (particularly the colon, rectum, or anus) or sexual organs
Medical Comorbidities Associated With Necrotizing Fasciitis Deaths in the United States
- Diabetes mellitus: 21%
- Other forms of heart disease: 20%
- Renal failure: 16%
- Other diseases of the respiratory system: 10%
- Mental and behavioral disorders due to psychoactive substance use: 10%
- Ischemic heart diseases: 8%
- Hypertensive diseases: 7%
- Diseases of the liver: 6%
- Obesity and other hyperalimentation: 5%
- Chronic lower respiratory diseases: 3%
- Influenza and pneumonia: 3%
- Metabolic disorders: 3%
- Malignant neoplasms of digestive organs: 3%
- Malignant neoplasms, stated or presumed to be primary, of lymphoid, hematopoietic, and related tissue: 3%
This is brought to you by NYRequirements.com's Training Certificates for OCFS and LDSS and New York State Infection Control and Barrier Precautions Training Course.